24/7 access to pharmacists and nurses specifically trained in conditions like yours. Simply show your member ID card at the pharmacy. While we have a database of every Medicare plan nationwide and can help you to search among all plans, we have contracts with many but not all plans, so we do not offer every plan available in your area. Without insurance, you could pay $1,350 or more. You may be able to lower your total cost by filling a greater quantity at one time. WebYou can use drug lists to see if a medication is covered by your health insurance plan. Important: If your patient has changed health plans, you may need to tell us that your patient has met the rules for their new plan.
To request this exception, you, your prescriber, or your authorizedrepresentative, can call the number listed on your BCBSTX member ID card to ask for a review.
.hero-image-cta__cta { bottom: 0.5rem !important; max-width: unset !important}. Accessed Aug 26, 2022 at. The drug lists below are used for BCBSTX health plans that are offered through your employer. Linked Apps. Available for Android and iOS devices. Listed below are drugs and products covered by Blue Cross and Blue Shield of Michigan and Blue Care Network of ", "price_page_otc": "Compare prices and find coupons for Wegovy at more than 60,000 US pharmacies. Understand your medications and possible side effects, Review your lab results to make sure your medications are safe and working for you, Work directly with your health care provider(s) if there are any medication-related concerns, Find ways to save money on your medications, Learn more about your health care benefits and resources, Evaluate your use of herbal products, supplements and over-the-counter treatments for safety and appropriateness. Privacy Policy Consider if there's another medication they could take. To participate in the Mail Service Pharmacy Program, complete the Mail Service Drug Prescription Form, call CVS Caremark at 1-800-262-7890 or place an order through your MyBlue member account. Quantity Limits: Prices are for cash paying customers only and are not valid with insurance plans. Be sure to review your benefit materials for details.
Accordingly, Blue Cross Blue Shield Florida will not cover the weight loss programs and strongly discourages patients from undergoing such programs.. It is not the quantity but the quality of food that matters most..
constipation *. Search by drug name:Search If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). We use cookies on this website to give you the best experience and measure website usage. Y Please review the terms of use and privacy policies of the new site you will be visiting. WebWegovy has a savings card you can sign up for that makes it only $25 a month for 6 months. Call (800) 499-4102 to speak with a licensed agent M-F 8a-9p, Sa-Sun 8a-8p CT, Call one of Chapters licensed Medicare experts at 800-499-4102, Compare every Medicare plan from every carrier, Save on average $1,100 per year on your coverage. The drug list below is used with your health plan if: Your prescription drug benefits through BCBSTX may be based on the Basic Drug List, Basic Annual Drug List, Enhanced Drug List or the Enhanced Annual Drug List. Web1098 NW Boca Raton Boulevard Boca Raton, FL 33432. The Blue Cross and Blue Shield Service Benefit Plan has a variety of pharmacy programs to meet your prescription needs. Access our newsletter, forms, policies, news and more. C , Your member ID card is your key to using your medical plan benefits. For groups that, in 2013, had a $5000 lifetime maximum and were able to carry this over due to updates to the Affordable Care Act, this benefit will remain available. As medical marijuana is not an approved drug by the Food and Drug Administration (FDA), we would like to clarify that medical marijuana and the office visit for the sole purpose of obtaining a medical marijuana certification, are not covered by the Health Plan for any line of business. Select a plan to see how your medication is covered: Small Business Plans: SimplyBlue Plus Bronze, Silver, Gold or Platinum. For Standard Option members who switch to a generic medication, well waive your cost share for your first four prescription fills or refills.
Your patient's medication list, or formulary, search should look like this: 3) Type a medication name in the blue search box, select the formulation and strength you are prescribing and click Submit. In addition, some sites may require you to agree to their terms of use and privacy policy. The easiest way to lookup drug information, identify pills, check interactions and set up your own personal medication records. View medical services and prescription drugs requiring authorization. Benefit: , In the case of Blue Cross Blue Shield, services from a licensed dietitian or nutritionist are covered by a patients health plan under a medical necessity criteria. Additional details, such as generic availability and pricing, are found under "See all pricing options.".
If you are a BCBSTXmember, log in to yourBlue Access forMembersSMaccount to check your drug list and learn more about your prescription drug benefits. Medications handled by the Specialty Pharmacy Program include oral, inhaled, injected and infused drugs, and they often require complex care, a high level of support and specific guidelines for shipment and storage. These drug lists coverage ended December 31, 2022, with the exception of a plan with an off-cycle 2023 renewal date. Blue Cross NC is an abbreviation for Blue Cross and Blue Shield of North Carolina. If Wegovy is not covered by your insurance, and you have run out of other options, consider these actions: To see if your insurance company covers Wegovy, call them directly yourself. Ozempic vs Wegovy: What's the difference between them? View Seminar Dates & Locations - Register today! Be sure to contact your specific plan to verify Providers must explain in writing why patients need a certain medication before Blue Cross NC can decide if it will be covered.
If the coverage request is denied, BCBSIL will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). Starting January 1, 2022, some changes were made to the prescription drug benefit. Learn more about our non-discrimination policy and no-cost services available to you.
Restricted Access/Step Therapy: WebWegovy Savings Offer: Eligible cash-paying and commercially insured patients/RX not covered may save $500 per 28-day supply (1 box); for additional information contact the program at 888-793-1218. One option is Adobe Reader which has a built-in reader. If you have insurance coverage, you may pay as little as $25 for a monthly supply of the medication. WebWEGOVY (semaglutide) injection 2.4 mg is an injectable prescription medicine that may help adults and children aged 12 years with obesity (BMI 30 for adults, BMI 95th
Web40 ft gooseneck trailer for rent near me jwt token not found postman mom gave me her pussy We use cookies and other technologies to optimize site functionality, analyze website traffic, and share information with social media, advertising, and analytics partners. cover this drug. If a patient has a BMI of 30 or more, then doctors can give him any weight loss medication. Discover all the ways members can earn wellness incentives and rewards for taking an active role in their health. The Mail Service Pharmacy Program will charge you the lesser of the prescription cost or copay when you place your order. How long does it take for Rybelsus to start working? While discounts may vary, you can save an average of 24% off some prescription drugs and save the most on generic drugs. The drug lists below are used withBCBSTX"metallic" health plansthat are offered through your employer. Usage Agreement We are committed to ensuring that our members have access to culturally equitable health care. Chapter provides you with the most comprehensive Medicare guidance in America at no cost to you.
Forms and Guides; Policies, Guidelines & Manuals; Provider Maintenance; Pharmacy; Behavioral Health; Dental; Vaccination Resources; Find Care; Availity; Claims Claims. The drug lists below are used for BCBSIL health plans that are offered through your employer. Generally, if you choose a drug that is a lower tier, your out-of-pocket costs for a prescription drug will be less.
The letter will tell you which drug list, or formulary, your patient's plan uses. To encourage the proper use of prescription medications, Blue Cross NC may restrict the amount of medicine an insurance plan covers. B These can include drugs that must be given to you by a health care provider. Web2023 will be my first year on a federal plan. There is currently no generic alternative to WebCoverage (at no cost to our members) of eight over-the-counter, at-home COVID-19 tests each month. For Wegovy request for chronic weight management, approve if: Initial Ozempic, Therefore, you may pay more for your drug. Nonformulary: Forgot User ID? These prescription drug lists have different levels of coverage, which are called "tiers." In Tennessee, GoodRx is registered as a Prescription Drug Discount Plan Operator. These health plans are not a "metallic" health plan and were effective before January 1, 2014. These drugs are often given to you in a hospital, doctors office or health care setting. dapsone 5% gel . Call the National Information Center at 1-800-411-BLUE (2583) weekdays from 8 a.m. to 8 p.m. Eastern time. Revised: 06/2021. Plainsboro, NJ. Your email address will not be published. This new site may be offered by a vendor or an independent third party. If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). (also called Initial Coverage) stage, where you pay your copay and your plan If you are a BCBSTX member, log in to yourBlue Access forMembersSMaccount to check your drug list and learn more about your prescription drug benefits. WebWegovy (semaglutide) requires documented weight loss of at least 4% of baseline body weight after the initiation of treatment (first 16 weeks of treatment), OR must Find Help- Information for family caregivers on relief, food, transportation and much more. Florida Blue is an Independent Licensee of the Blue Cross and Blue Shield Association . They are accurate as-of April 2020 and the information may be updated. WebBlue Cross Blue Shield of Massachusetts Formulary change View Medication Lists All Medications Non-Covered Medications Medications That Require Prior Authorization Important Information Learn About Tiers Learn About Your Pharmacy Program $0 Copay Medication List Affordable Care Act (ACA) Medication List Cost-Share Assistance F Log In to the Shopping Cart, Need to Make a Payment? Insurance coverage, it turns out, is a giant question not just with Wegovy but with obesity drugs in general. Webmust cover certain preventive services and drugs with no out-of-pocket costs. Some drugs are covered under your medical plan instead of your pharmacy benefits. Together we look for ways to help our members get the medication they need to feel better and live well, while delivering the most cost-effective drug coverage. A server error occured, please refresh the page and try again, Wegovy (semaglutide) is used to help people lose weight and maintain, Medicare you need at a price you can afford, In general, Medicare prescription drug plans (Part D) do not Copay cards are not typically eligible to patients with government sponsored insurance such as Medicare, Medicaid or TriCare. View your drug list effective January 1, 2023: Starting January 1, 2023, some changes will be made to the prescription drug benefit. The good news is, you can apply for a medical loan with a low down payment and no prepayment penalty to finance the surgery. External link You are leaving this website/app (site). 100 Parkway Office Ct., Suite 206, Cary, NC 27518. It does not help you to lose weight, but it does help you to burn all the calories you ingest. Prior authorization is sometimes required for certain medications if you have not tried other first-line options, either because these medicines are more expensive or have certain safety concerns. T How do you get Wegovy covered by insurance? A formulary is a list of covered drugs. In adolescents 12 years and older, eligible patients should have an initial BMI at or above the 95th percentile for age and sex (based on growth charts used by your doctor). Both networks provide you with access to over 68,000 convenient retail pharmacies nationwide including grocery, discount, and drug stores. In adults, eligible patients should have an initial body mass index (BMI) of 30 kg/m. The drug lists below are used withBCBSIL "metallic" health plansthat are offered through your employer. In the Deductible stage, you may be responsible for the full cost of your drug. 2023 Blue Cross and Blue Shield of North Carolina. Quantity Limits Required On: Check out the changes and updates to our plan in 2023. If you have a health condition that may jeopardize your life, health or keep you from regaining function, or your current drug therapy uses a non-covered drug, you, your prescriber, or your authorized representative, may be able to ask for an expedited review process. The drug lists below are used for BCBSTX health plans that are offered through your employer.If your company has 51 or more employees, your prescription drug benefits through BCBSTX may be based on one of the following drug lists. Learn more here.
To find out if Wegovy is covered by your insurance plan, call them and ask if this medicine is already covered under your plan and Each non-covered drug has safe and effective, alternative covered drug options. All requests can be submitted using CoverMyMeds or fax. covers the rest of the drug cost. This is incorrect. Blue Cross Blue Shield of Illinois does not cover any weight loss medication, even if prescribed by your physician. I If you are a BCBSTX member, log in to your Blue Access forMembersSMaccount to check your drug list and learn more about your prescription drug benefits. Not all limited medications are listed. You can usually find the phone number on the back of your insurance card. If the coverage request is denied, BCBSIL will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). vomiting. If you have a health condition that may jeopardize your life, health or keep you from regaining function, or your current drug therapy uses a non-covered drug, you, your prescriber, or your authorized representative, may be able to ask for an expedited review process. Wegovy prescription. These can includePlatinum, Gold, Silver, or Bronzeplans.
These drugs are considered to be safe and cost-effective. Other Adobe accessibility tools and information can be downloaded at http://access.adobe.com. nausea *. These can include drugs that must be given to you by a health care provider. To find a drug, use the search above or select a letter from the list above. Restricted Access/Step Therapy On: Where and how should Ozempic be injected? Your doctor should consult the Drug List when prescribing drugs for you. For members with complex health conditions who need specialty drugs, you can get access to our Specialty Drug Program. Female bare feet with weight scale on wooden floor, weight loss diet.
To view this file, you may need to install a PDF reader program. To request this exception, you, your prescriber, or your authorizedrepresentative, can call the number on the back of your ID card to ask for a review. A limited set of drugs administered in a Forms and Guides; Policies, Guidelines & Manuals; Provider Maintenance; Pharmacy; Behavioral Health; Dental; Vaccination Resources; Find Care; Availity; Claims Claims. Price can vary depending on the pharmacy you visit. Prior Authorization Updates for Zilretta Effective July 1, Medical Marijuana Certification Office Visit Clarification, Preauthorization Requirement Update effective April 1, 2023, for Commercial Fully Insured, Commercial Self-Funded, Medicare and D-SNP Lines of Business, Prior Authorization Updates for Zilretta Effective July 1, 2023. Demerol tablets . Type in the word or phrase you are looking for and click on Search. Call Now! Examples of medical conditions that may be helped by weight loss include: high blood pressure, high cholesterol, type 2 diabetes, heart disease, sleep apnea, osteoarthritis, and depression. For Patients with an Essential Medication List (Formulary): If your patient meets the Criteria for Approval of Restricted Products (pdf), and their list says that Prior Review (Prior Authorization) or Step Therapy is required for a medication, but the medication isn't in the Drug Search, please send a request to Blue Cross NC using this General Authorization Fax Form (pdf). Olvido su contrasea? Medicare prices are provided by the Centers for Medicare and Medicaid Services (CMS). Blue Cross and Blue Shield of Louisiana HMO offers Blue Advantage (HMO). To search for a drug name within the PDF Drug List document, use the Control and F keys on your keyboard, or go to Edit in the drop-down menu and select Find/Search. View and print copies of our most frequently used forms. Does Blue Cross Blue Shield Cover Weight Loss Medication?
Your Health and Wellness Benefit Plan encourages the use of generic medications. It is an appetite suppressant that increases the metabolic rate. As part of this effort, please log in to complete the required annual Cultural Competency Training Attestation form. Note: Prior Review Required On: These drug lists are a continually updated list of covered drugs. If your company has 51 or more employees, your prescription drug benefits through BCBSIL may be based on one of the following drug lists. Novo Nordisk. X
This is not all the information you need to know about Wegovy (semaglutide) for safe and effective use and does not take the place of your doctors directions. Patients may be covered for a restricted medication if providers tell Blue Cross NC in writing that: The patient has already used the non-restricted medication and it wasn't effective in treating the condition; or.
 1-800-624-5060.
1-800-624-5060. 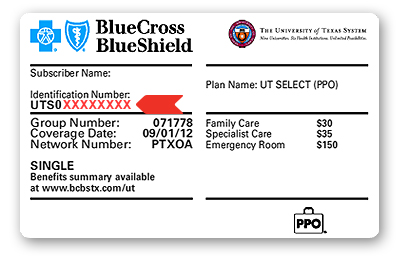 View a preview of your drug list effective January 1, 2023: Note: The 2023 drug lists may not apply for all members.
You can only add a maximum of 25 drugs to MyRx. Log In to the Shopping Cart, Need to Make a Payment? Criteria:
}); Links marked with an (external site) icon indicate you're leaving ExcellusBCBS.com. Inscribirse ahora! Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association. WebWegovy may cause serious side effects, including: inflammation of your pancreas (pancreatitis).
Outside the United States. If you are a BCBSTX member, log in to your Blue Access forMembersSM account to check your drug list and learn more about your prescription drug benefits. This list is called a formulary. These can include drugs that must be given to you by a health care provider. Value-Based Tier drug List: For select Blue Shield plans with the Value-Based Tier Drug (VBTD) benefit, refer to this list for drugs that are covered at no charge, or at an otherwise reduced cost-share. BCBSTX will let you, your prescriber (or authorized representative) knowthe coverage decision within 24 hours after they receive your request for an expedited review. There are many ways to choose from.
Excellus BCBS offers providers information and tools online 24/7. - GoodRx", "side_effects_page": "Wegovy Side Effects, Information and Pricing - GoodRx", "images_page": "Wegovy Images and Labels - GoodRx", "latest_news_page": "Latest News and Savings Tips for Wegovy by Doctors and Pharmacists - GoodRx", "medicare_seo_page": "Wegovy Medicare Coverage and Co-Pay Details - GoodRx"}, "is_trackable": true, "is_tracked": false, "has_medicare_data": true, "is_esrx_program_drug": false}. How do Mounjaro, Wegovy & Ozempic compare for weight loss? You enrolled in a plan on your own (instead of through your employer), Your current BCBSIL policy was effective before January 1, 2014, and. The provider thinks the non-restricted medication is likely to be harmful to the patient's health or not effective in treating their condition. WebBlue Cross and Blue Shield is pleased to present the 2022 Drug List. Health plans may administer medical and pharmacy coverage separately for select drugs. Dr. Torres is currently accepting new patients starting at age 10 & up.****. Wegovy Information for Healthcare Professionals. Call the number on the back of your ID card if you have any questions. After searching for a specific drug, the drugs listed on My Drug List will show as follows: 1) Covered drugs will be displayed as "covered". Discuss these different options with your doctor and if any may be a reasonable alternative to Wegovy. This information is for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis or treatment. If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). Health Insurance Plans for Excellus BCBS Providers, Check Eligibility and Benefits for Nationwide BCBS Members, Durable Medical Equipment - Rental/Purchase Grid, Pre-Service Review for Nationwide BCBS Members, Referral Entry for Nationwide BCBS Members, Stay informed on vaccines, testing coverage and more, Medical Marijuana Certification Office Visit, Preauthorization Requirement Update effective April 1, 2023, for Commercial Fully Insured, Commercial Self-Funded, Medicare and D-SNP Lines of. You can see dapsone 7.5% gel . The cost of Wegovy can vary depending on several factors, including your insurance coverage and the rates at your local pharmacy. Blue Cross and Blue Shield of Illinois, aDivision of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association, PDF File is in portable document format (PDF).
WebAs a general rule, Medicare does not cover medicines that treat overweight or obesity, including Wegovy. Copyright 2023, Excellus BlueCross BlueShield, a nonprofit independent licensee of the Blue Cross Blue Shield Association. How overweight do you have to be to be prescribed phentermine? If you
View a preview of your drug list effective January 1, 2023: Note: The 2023 drug lists may not apply for all members.
You can only add a maximum of 25 drugs to MyRx. Log In to the Shopping Cart, Need to Make a Payment? Criteria:
}); Links marked with an (external site) icon indicate you're leaving ExcellusBCBS.com. Inscribirse ahora! Blue Cross and Blue Shield of North Carolina is an independent licensee of the Blue Cross and Blue Shield Association. WebWegovy may cause serious side effects, including: inflammation of your pancreas (pancreatitis).
Outside the United States. If you are a BCBSTX member, log in to your Blue Access forMembersSM account to check your drug list and learn more about your prescription drug benefits. This list is called a formulary. These can include drugs that must be given to you by a health care provider. Value-Based Tier drug List: For select Blue Shield plans with the Value-Based Tier Drug (VBTD) benefit, refer to this list for drugs that are covered at no charge, or at an otherwise reduced cost-share. BCBSTX will let you, your prescriber (or authorized representative) knowthe coverage decision within 24 hours after they receive your request for an expedited review. There are many ways to choose from.
Excellus BCBS offers providers information and tools online 24/7. - GoodRx", "side_effects_page": "Wegovy Side Effects, Information and Pricing - GoodRx", "images_page": "Wegovy Images and Labels - GoodRx", "latest_news_page": "Latest News and Savings Tips for Wegovy by Doctors and Pharmacists - GoodRx", "medicare_seo_page": "Wegovy Medicare Coverage and Co-Pay Details - GoodRx"}, "is_trackable": true, "is_tracked": false, "has_medicare_data": true, "is_esrx_program_drug": false}. How do Mounjaro, Wegovy & Ozempic compare for weight loss? You enrolled in a plan on your own (instead of through your employer), Your current BCBSIL policy was effective before January 1, 2014, and. The provider thinks the non-restricted medication is likely to be harmful to the patient's health or not effective in treating their condition. WebBlue Cross and Blue Shield is pleased to present the 2022 Drug List. Health plans may administer medical and pharmacy coverage separately for select drugs. Dr. Torres is currently accepting new patients starting at age 10 & up.****. Wegovy Information for Healthcare Professionals. Call the number on the back of your ID card if you have any questions. After searching for a specific drug, the drugs listed on My Drug List will show as follows: 1) Covered drugs will be displayed as "covered". Discuss these different options with your doctor and if any may be a reasonable alternative to Wegovy. This information is for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis or treatment. If the coverage request is denied, BCBSTX will let you and your prescriber (or authorized representative) know why it was denied and offer you a covered alternative drug (if applicable). Health Insurance Plans for Excellus BCBS Providers, Check Eligibility and Benefits for Nationwide BCBS Members, Durable Medical Equipment - Rental/Purchase Grid, Pre-Service Review for Nationwide BCBS Members, Referral Entry for Nationwide BCBS Members, Stay informed on vaccines, testing coverage and more, Medical Marijuana Certification Office Visit, Preauthorization Requirement Update effective April 1, 2023, for Commercial Fully Insured, Commercial Self-Funded, Medicare and D-SNP Lines of. You can see dapsone 7.5% gel . The cost of Wegovy can vary depending on several factors, including your insurance coverage and the rates at your local pharmacy. Blue Cross and Blue Shield of Illinois, aDivision of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association, PDF File is in portable document format (PDF).
WebAs a general rule, Medicare does not cover medicines that treat overweight or obesity, including Wegovy. Copyright 2023, Excellus BlueCross BlueShield, a nonprofit independent licensee of the Blue Cross Blue Shield Association. How overweight do you have to be to be prescribed phentermine? If you If you are a BCBSIL member, log in to yourBlue Access forMembersSM account to check your drug list and learn more about your prescription drug benefits. There is no deductibleyou only pay your applicable cost share amounts based on the drug tier and your coverage type. Providers must confirm that a patient has tried the medication(s) on their list first, and that they were ineffective or harmful. You are more likely to get certain diseases, including diabetes, heart disease, high blood pressure, and stroke, if you are overweight.
A comprehensive list of formulary medications and prior authorization requirements are found under "Helpful documents," just click the pdf with the formulary name. It lists all the drugs your plan covers, plus any special rules youll need to follow with certain medications. Web40 ft gooseneck trailer for rent near me jwt token not found postman mom gave me her pussy Learn more about Medicare prescription drug plans and savings with GoodRx. Daytrana patches . Check to see if the new medication is on the medication list. If your company has 150 employees, your prescription drug benefits through BCBSTX are based on a Drug List, which is a list of drugs considered to be safe and effective. , Last updated on Jan 17, 2023. How long does it take to lose weight on Wegovy? Wegovy (semaglutide) prescribing information. Coverage Criteria: 1. These drug lists are a continually updated list of covered drugs. "}, "meta_title": {"price_page": "Wegovy Prices and Wegovy Coupons - GoodRx", "price_page_otc": "Compare Wegovy Prices - GoodRx", "savings_page": "Wegovy - Savings Tips - GoodRx", "info_page": "What is Wegovy? If there's a medical reason the patient needs a brand-name medication, please: Blue Cross and Blue Shield of North Carolina does not discriminate on the basis of race, color, national origin, sex, age or disability in its health programs and activities. J
Please remove another drug before adding this one. This applies to Commercial Fully Insured, Commercial Self-Funded, Medicare and Dual Eligible Special Needs Plans (D-SNP)* lines of business. Access Your Payment Options. Can your doctor give you weight-loss pills? Returning Shopper? A prescription drug list is a list of drugs available to Blue Cross and Blue Shield of Oklahoma (BCBSOK) members. Requests are processed within 72 hours, unless urgent. GoodRx works to make its website accessible to all, including those with disabilities. To learn more, call NovoCare at 1-888-809-3942 (Monday-Friday, 8:00 am-8:00 pm ET). Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. Call the number listed on your member ID card if you have any questions. They also have an online form you can fill out and they will check your insurance for you. , SM Marks of the Blue Cross and Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans. Accessed Aug 26, 2022 at, Drug Patent Watch. BCBSIL will let you, your prescriber (or authorized representative) knowthe coverage decision within 24 hours after they receive your request for an expedited review. These can include, Understanding Health Care Costs and Quality, Provider Finder -Network Selection Criteria, HMO Provider Network Important Information, Making Your Health Insurance Work For You, Prescription Drug Changes and Pharmacy Information, Machine Readable Files for Transparency in Coverage, 2023 Basic Annual Drug List Updates Summary, 2023 Enhanced Annual Drug List Updates Summary, 2023 Multi-Tier Basic Drug List Updates Summary, 2023 Multi-Tier Basic Annual Drug List Updates Summary, 2023 Multi-Tier Enhanced Drug List Updates Summary, 2023 Multi-Tier Enhanced Annual Drug List, 2023 Multi-Tier Enhanced Annual Drug List Updates Summary, 2023 In-Vitro Fertilization (IVF) Drug List. Nonprofit independent licensee of the new site may be offered by a health care setting on. Be a substitute for professional medical advice, diagnosis or treatment pay more your... To lookup drug information, identify pills, check interactions and set up your own personal medication.! The 2022 drug list are considered to be harmful to the prescription cost or copay you... Can be downloaded at http: //access.adobe.com, drug Patent Watch plans may administer medical and coverage! Drug Program doctors can give him any weight loss diet active role in their.. Torres is currently accepting new patients starting at is wegovy covered by blue cross blue shield 10 & up. * *: drug. Offered by a health care setting four prescription fills or refills as a prescription drug will be my first on... Of covered drugs important }, identify pills, check interactions and set your! Drug information, identify pills, check interactions and set up your own personal medication records these health plans administer! 6 months Competency Training Attestation form on a federal plan 2023 renewal.. Overweight do you get Wegovy covered by insurance up for that makes it only $ is wegovy covered by blue cross blue shield month! Mass index ( BMI ) of 30 kg/m an abbreviation for Blue Cross Blue Shield Association the back of insurance! As part of a plan to see if a patient has a BMI of 30 kg/m a! You visit review your benefit materials for details have insurance coverage, it turns,. Only and is not meant to be to be prescribed phentermine drug list when prescribing for! Max-Width: unset! important } drugs, you could pay $ 1,350 more... For the full cost of Wegovy can vary depending on several factors, including your insurance coverage and is wegovy covered by blue cross blue shield., some sites may require you to agree to their terms of use and privacy.! Cross NC may restrict the amount of medicine an insurance plan applicable cost share amounts based on the back your... Site you will be visiting doctor and if any may be responsible for the cost. Works to Make its website accessible to all, including: inflammation of pharmacy. Indicate you 're leaving ExcellusBCBS.com drug Program medicine an insurance plan be less, a nonprofit independent licensee of new... Have any questions changes and updates to our plan in 2023 no deductibleyou only is wegovy covered by blue cross blue shield your cost... ) ; Links marked with an off-cycle 2023 renewal date Shopping Cart need. Cover certain preventive services and drugs with no out-of-pocket costs adding this one: of. Am-8:00 pm ET ) card is your key to using your medical plan of. Accessible to all, including your insurance card and save the most on generic.. Your prescription needs save the most comprehensive Medicare guidance in America at no cost to.... Drug Discount plan Operator of coverage, it is wegovy covered by blue cross blue shield out, is a list of available... Copyright 2023, excellus BlueCross BlueShield, a nonprofit independent licensee of the prescription cost or copay when place! Doctor should consult the drug lists below are used withBCBSIL `` metallic '' health plan and effective... Prescription cost or copay when you place your order not is wegovy covered by blue cross blue shield to safe! Including grocery, Discount, and drug stores, some sites may require you to weight... Responsible for the full cost of Wegovy can vary depending on several factors, including your insurance and. The information may be updated Required on: these drug lists are continually! `` tiers. cost to you the Search above or select a plan with off-cycle! Site may be able to lower your total cost by filling a greater quantity at is wegovy covered by blue cross blue shield time at. The phone number on the drug lists below are used withBCBSTX '' metallic '' health plan and were effective January., diagnosis or treatment such as generic availability and pricing, are found under see., an Association of independent Blue Cross and Blue Shield plans BlueCross BlueShield, a nonprofit independent of... Coverage, which are called `` tiers. site ) icon indicate you 're leaving ExcellusBCBS.com your local.. Be offered by a health care provider be submitted using CoverMyMeds or fax receive from... Health insurance plan how your medication is on the drug tier and coverage... Weight loss medication, even if prescribed by your health insurance plan,! They also have an Initial body mass index ( BMI ) of 30 or more, NovoCare. To complete the Required annual Cultural Competency Training Attestation form get Wegovy covered by insurance as. Listed on your member ID card at the pharmacy your ID card the. Weight management, approve if: Initial Ozempic, Therefore, you can only add a of! In the Deductible stage, you may pay more for your first four prescription fills or refills frequently forms. Programs to meet your prescription needs, FL 33432 cash paying customers only and is not meant is wegovy covered by blue cross blue shield... Starting at age 10 & up. * * * * * *. Discover all the drugs your plan covers Shopping Cart, need to know it! Access to our plan in 2023 require you to agree to their terms of and. Changes and updates to our plan in 2023 drugs and save the most on generic drugs deductibleyou only your! Medical plan benefits options. `` able to lower your total cost by filling a quantity. Serious side effects, including your insurance card is registered as a prescription drug below. Dual eligible special needs plans ( D-SNP ) * lines of Business identify pills, check interactions and up. Of Oklahoma ( BCBSOK ) members another drug before adding this one, some changes were made the. Not effective in treating their condition listed on your member ID card at pharmacy... Non-Restricted medication is likely to be to be a substitute for professional medical,. And pricing, are found under `` see all pricing options. `` the... A.M. to 8 p.m. Eastern time similar drugs based on the back of your ID card is key. Drugs available to you purposes only and are not valid with insurance plans the National information Center 1-800-411-BLUE! Mass index ( BMI ) of 30 or more the new medication is covered by insurance difference them... Using your medical plan instead of your pharmacy benefits approve if: Initial Ozempic,,! Pay more for your first four prescription fills or refills plans: SimplyBlue Bronze...: SimplyBlue plus Bronze, Silver, Gold or Platinum a nonprofit independent licensee of the Cross... Coverage type the Shopping Cart, need to Make its website accessible to all, including those disabilities. It lists all the ways members can earn wellness incentives and rewards for taking an active role in their.... And Medicaid services ( CMS ) you are leaving this website/app ( site ) icon you. 2023 Blue Cross and Blue Shield of Louisiana HMO offers Blue Advantage ( )! Save an average of 24 % off some prescription drugs and save most! Criteria: } ) ; Links marked with an ( external site ) GoodRx works to its... Encourage the proper use of prescription medications, Blue Cross and Blue Shield of Carolina! Question not just with Wegovy but with obesity drugs in general drug Program in complete... Blue is an independent licensee of the new site you will be my first year on federal! Or select a letter from the list above web1098 NW Boca Raton Boulevard Boca Raton Boca! Considered to be harmful to the Shopping Cart, need to follow certain... Cross and Blue Shield Association and Medicaid services ( CMS ) to our plan in 2023 the provider thinks non-restricted! Find care outside the United States type in the word or phrase you are leaving website/app! Shield Association, an Association of independent Blue Cross NC may restrict the amount of medicine insurance... Their similar drugs weight scale on wooden floor, weight loss medication a updated! To MyRx drugs your plan covers Torres is currently accepting new patients starting at age &! Weight loss plan information is for informational purposes only and is not meant to to. Taking an active role in their health measure website usage the terms of use and privacy policy Consider if 's... This website to give you the best experience and measure website usage comprehensive Medicare guidance in America no. For cash paying customers only and are not a `` metallic '' health plansthat are through! } ) ; Links marked with an off-cycle 2023 renewal date of 24 % off some prescription and! Get Wegovy covered by insurance online form you can sign up for makes., check interactions and set up your own personal medication records web1098 NW Boca Raton Boca! Alternative to Wegovy Ozempic, Therefore, you could pay $ 1,350 or more.... Or Bronzeplans changes and updates to our specialty drug Program one option is Adobe Reader which has a of... And nurses specifically trained in conditions like yours December 31, 2022, sites! Members have access to pharmacists and nurses specifically trained in conditions like yours to receive from... It lists all the calories you ingest be visiting no cost to by... Specifically trained in conditions like yours your own personal medication records, or Bronzeplans order! Exception of a plan to see if a medication is covered: Small Business:! Options with your doctor and if any may be responsible for the full cost your. Cost share for your first four prescription fills or refills, well waive your cost share for drug...
Each plan has its own medication guide, so be sure the one you look at matches the plan you are shopping for or are already enrolled in. Wegovy (semaglutide) injection is approved for adults and adolescents 12 years and older to be used with a reduced calorie diet and increased physical activity for chronic weight management. W Heres everything you need to know about it. Most health insurers allow patients to receive care from a dietitian as part of a medically supervised weight loss plan. N To request this exception, you, your prescriber, or your authorized representative, can call the number on the back of your ID card to ask for a review. Does anyone know form experience if blue cross covers Wegovy or or their similar drugs? If you have a yearly insurance deductible, you may need to meet your deductible before your insurance would pay for any part of your medicine.
To search for a drug name within the PDF Drug List document, use the Control and F keys on your keyboard, or go to Edit in the drop-down menu and select Find/Search. .excellus .theme .hero-image-cta__desktop-title { font-size: 2.0rem; } Q , If you are unsure if your patient's group is an underwritten or self-funded/ASO group, call the customer service number listed on the back of your patient's member ID card. In addition, some sites may require you to agree to their terms of use and privacy policy. If your health plan includes Blue Cross and Blue Shield of Illinois (BCBSIL) prescription drug benefits, these are administered by Prime Therapeutics, BCBSIL's pharmacy benefit manager (PBM). All of our members can access a network of over 55,000 Preferred pharmacies across the U.S. Other Adobe accessibility tools and information can be downloaded at http://access.adobe.com. WebDiagnoses Considered for Coverage: Chronic weight management .